- Vaginal delivery usually not possible
- Unless the child is small
- Twins
- Prematures.
- Deliver by C/S.
SPONTANEOUS VAGINAL DELIVERY

Looks awfull…. 
….but….. 
…..spontanous recovery is fast
BROW PRESENTATION
The Rebel Surgeon's personal experience from working in remote facilities with limited resources
SPONTANEOUS VAGINAL DELIVERY







BROW PRESENTATION



ALIVE FETUS
DEAD FETUS (IUFD)
Gestational age < 26 weeks
Gestationalage > 26 weeks
MAURICEAU-LEVRET
For delivering head at Breech Presentation



INTERNAL VERSION AND EXTRACTION
For delivering breech and transverse presentations
ARM RELEASE
In Assisted Breech Delivery
BURN-MARSHALL

LOEVSET
For delivering the shoulders

Painless – sometimes massive – bleeding in the last trimester of the pregnancy strongly suggests previa.
Same treatment whether fetus is alive or dead:
When ultrasound is not available
Watch out for signs of DIC (HELLP Syndrome). Transfuse with fresh blood at the slightest suspicion
PREMATURE CONTRACTIONS
INSUFFICIENT CERVIX





PREMATURE DELIVERY






When presenting twin (twin A) is in breech and second twin (twin B) in a cephalic presentation there is a risk of “locked twins”. In this case deliver by C/S

VAGINAL DELIVERY – both twins in breech















RETAINED TWIN B
Cervix is fully dilated
Cervix is not fully dilated
LOCKED TWINS
Head of second twin (twin B) in cephalic presentation locks head of presenting twin (twin A) in breech. Chin against chin.
Both twins alive
First twin (twin A) is dead / Second twin (twin B) is alive


















Both twins dead
Same procedure as with “First twin dead / Second twin alive”
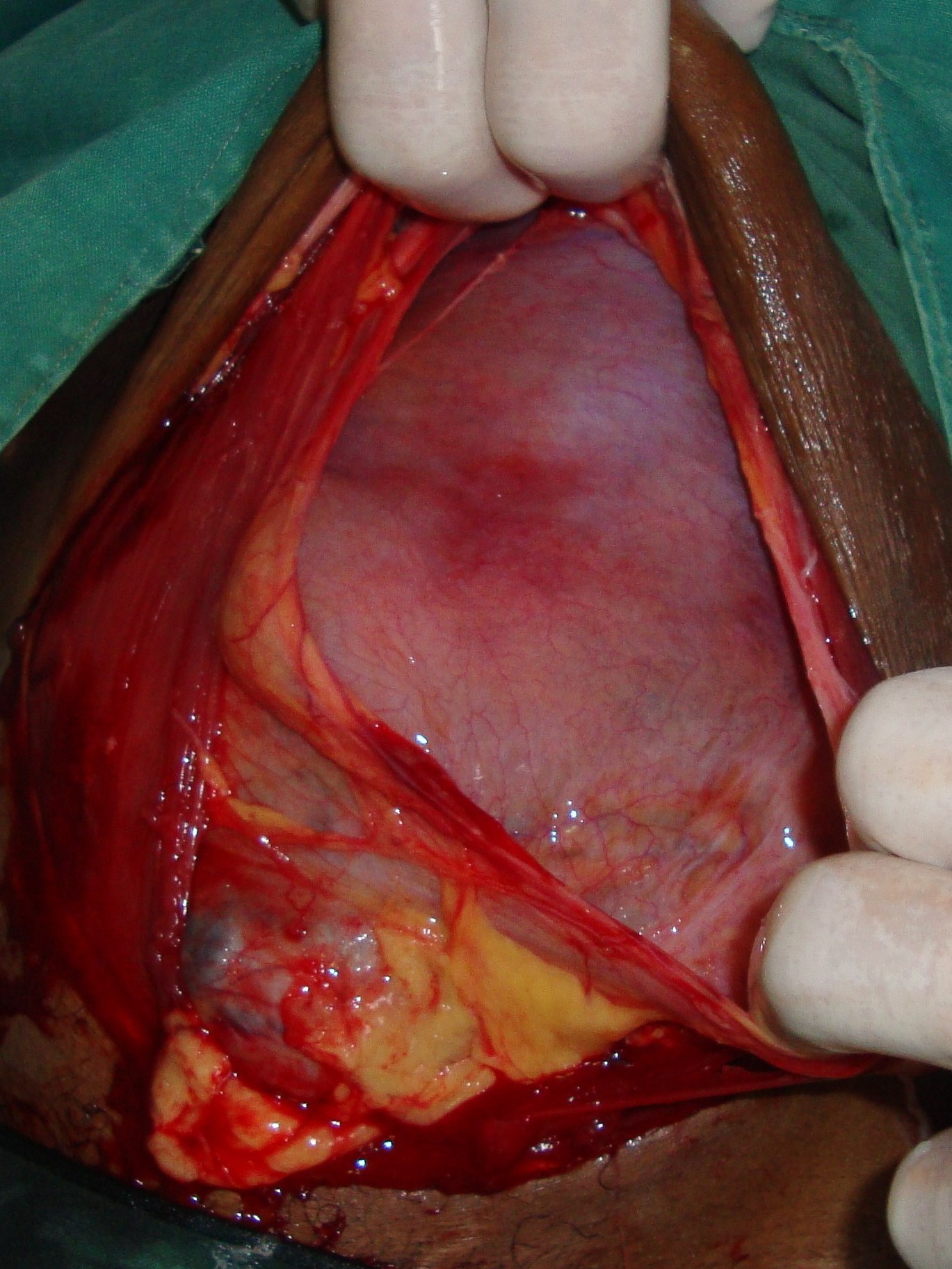
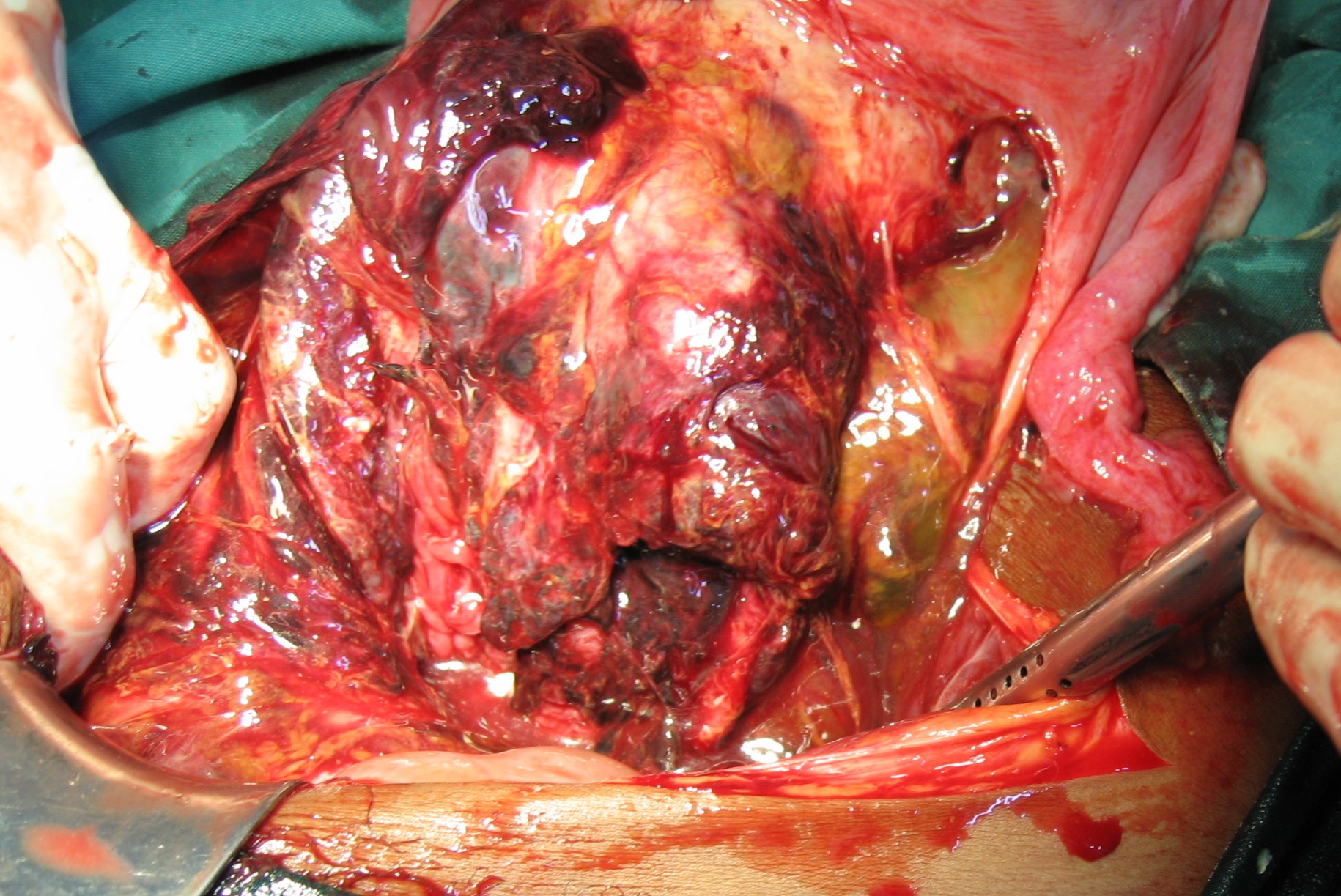
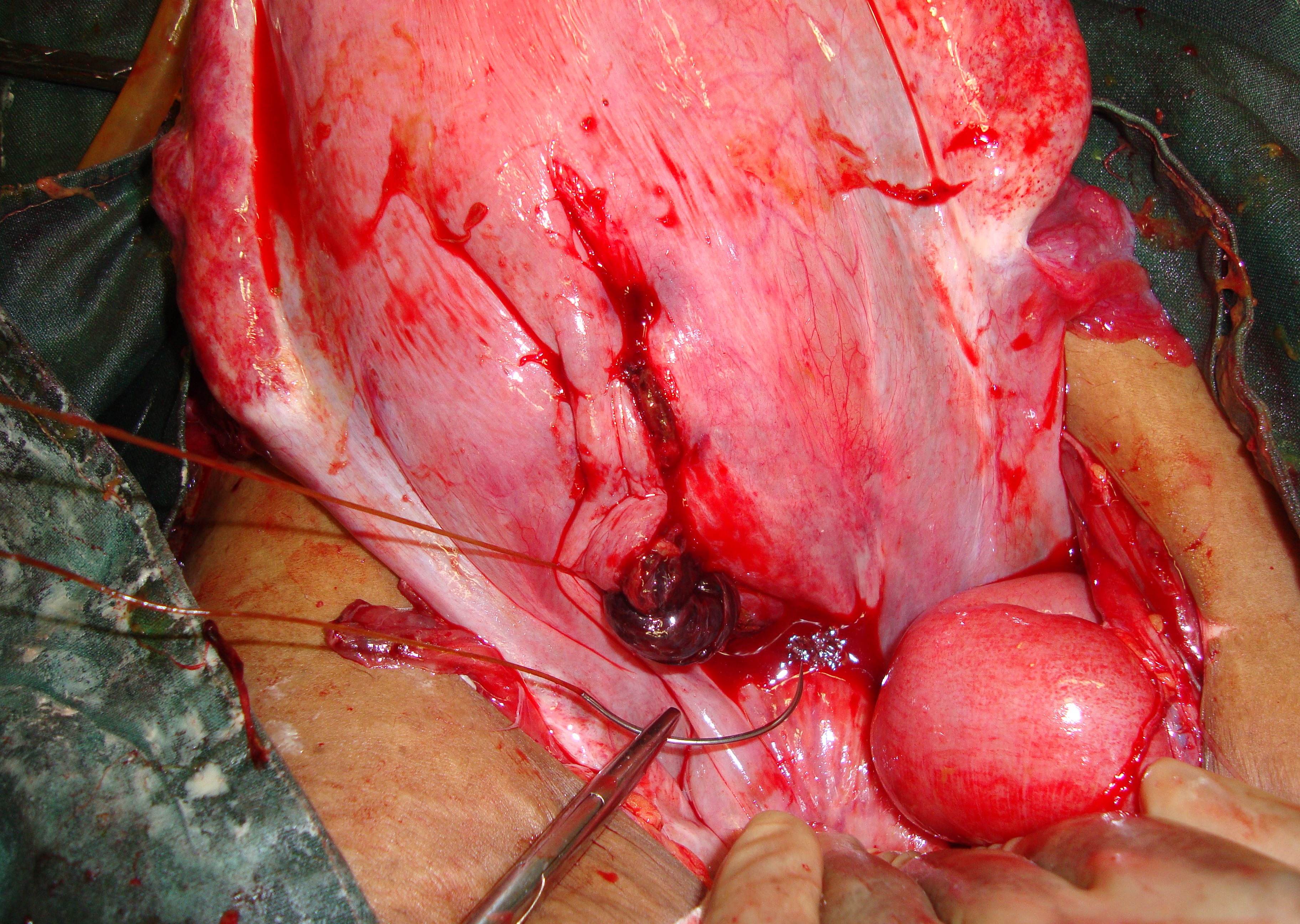
Ultimate result of unrelieved obstructive labor
Symptoms and signs
Diagnosis


If diagnosis is still in doubt, there are two options:
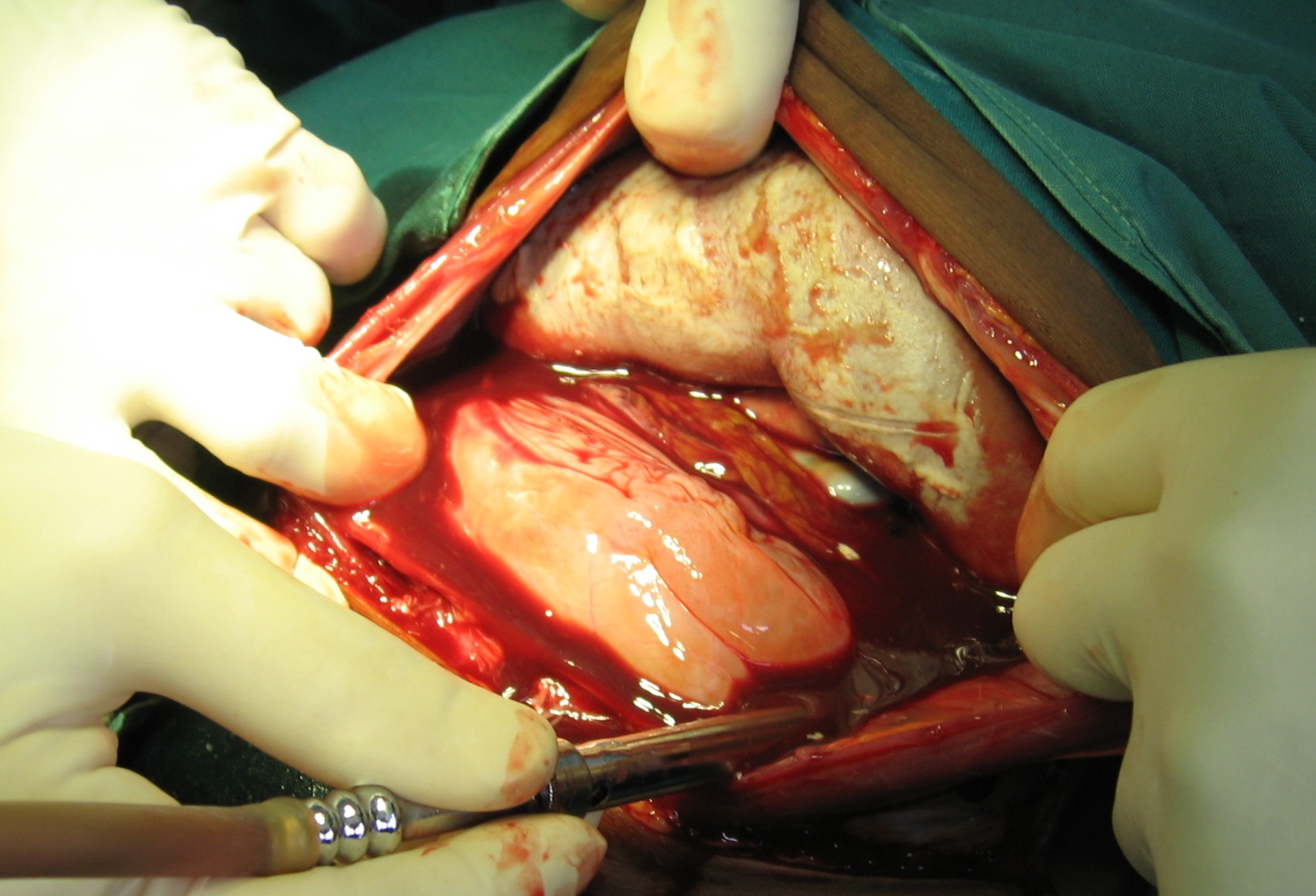
I. Do a laparotomy
Rupture is present:
No rupture is present:



II. Deliver the dead fetus by destructive procedure
Check uterine cavity manually for rupture
In selected cases, when:
TYPES of RUPTURES:
The far most common type is the anterior transverse.
Use the same principles as in trauma surgery:




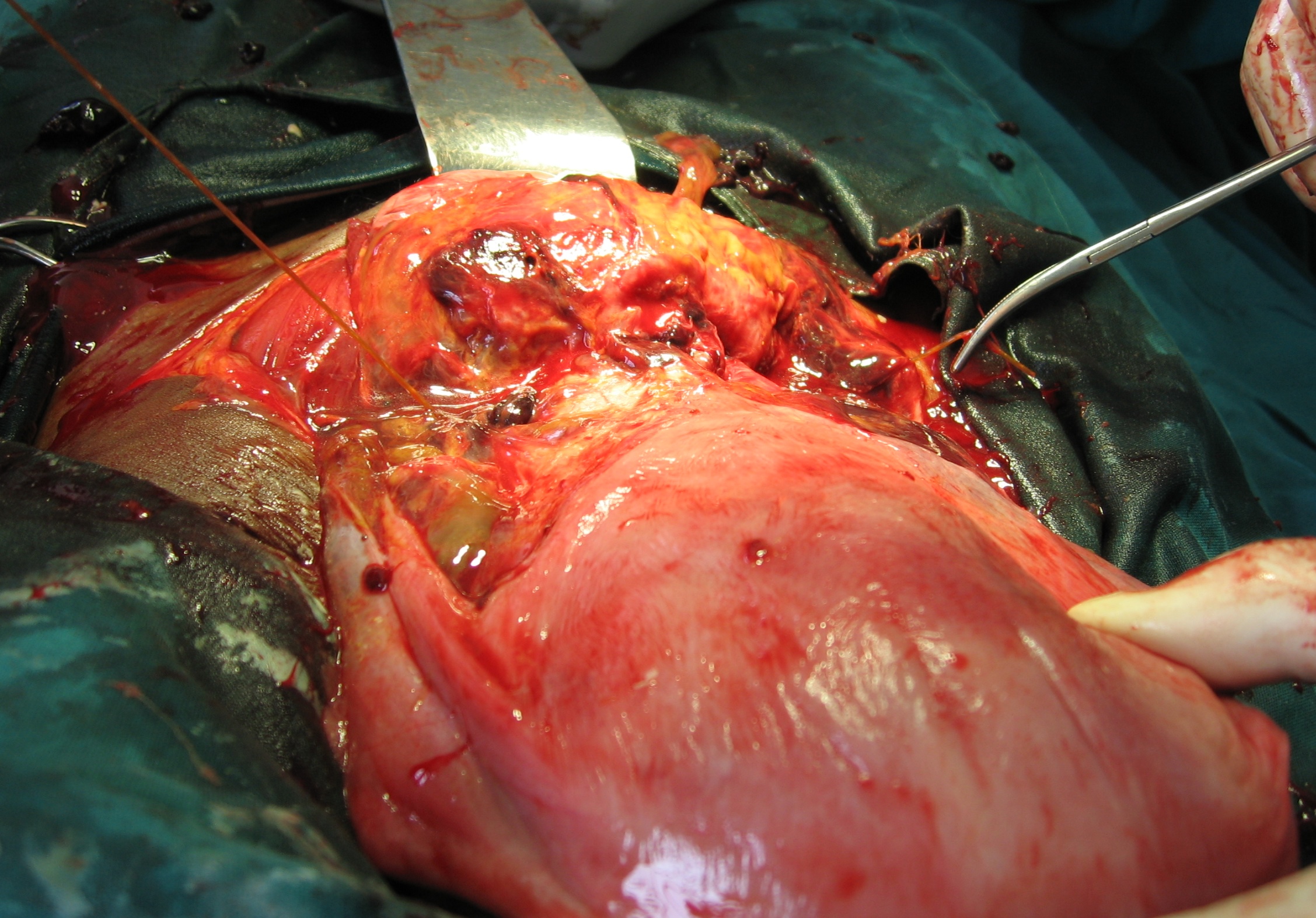
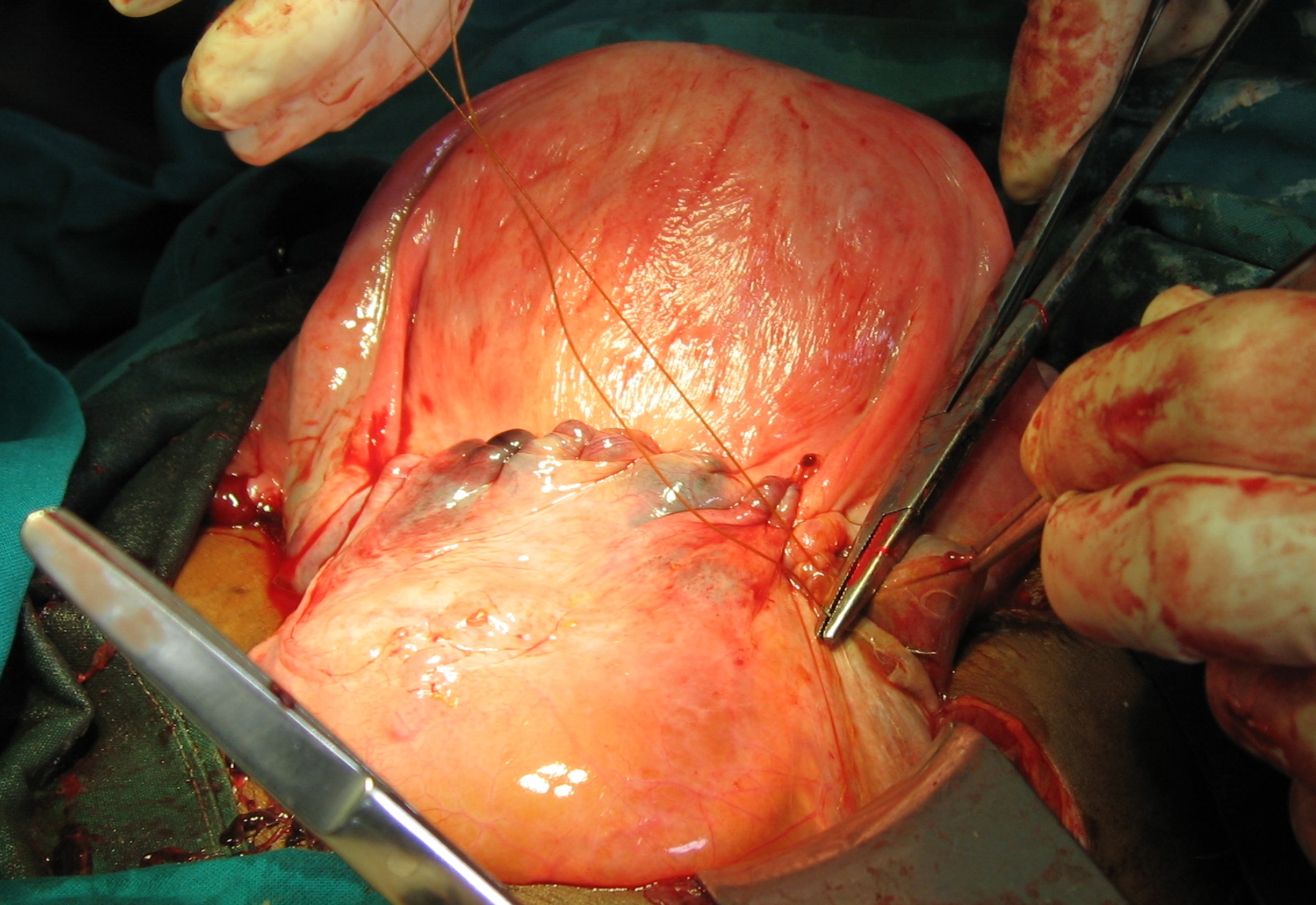
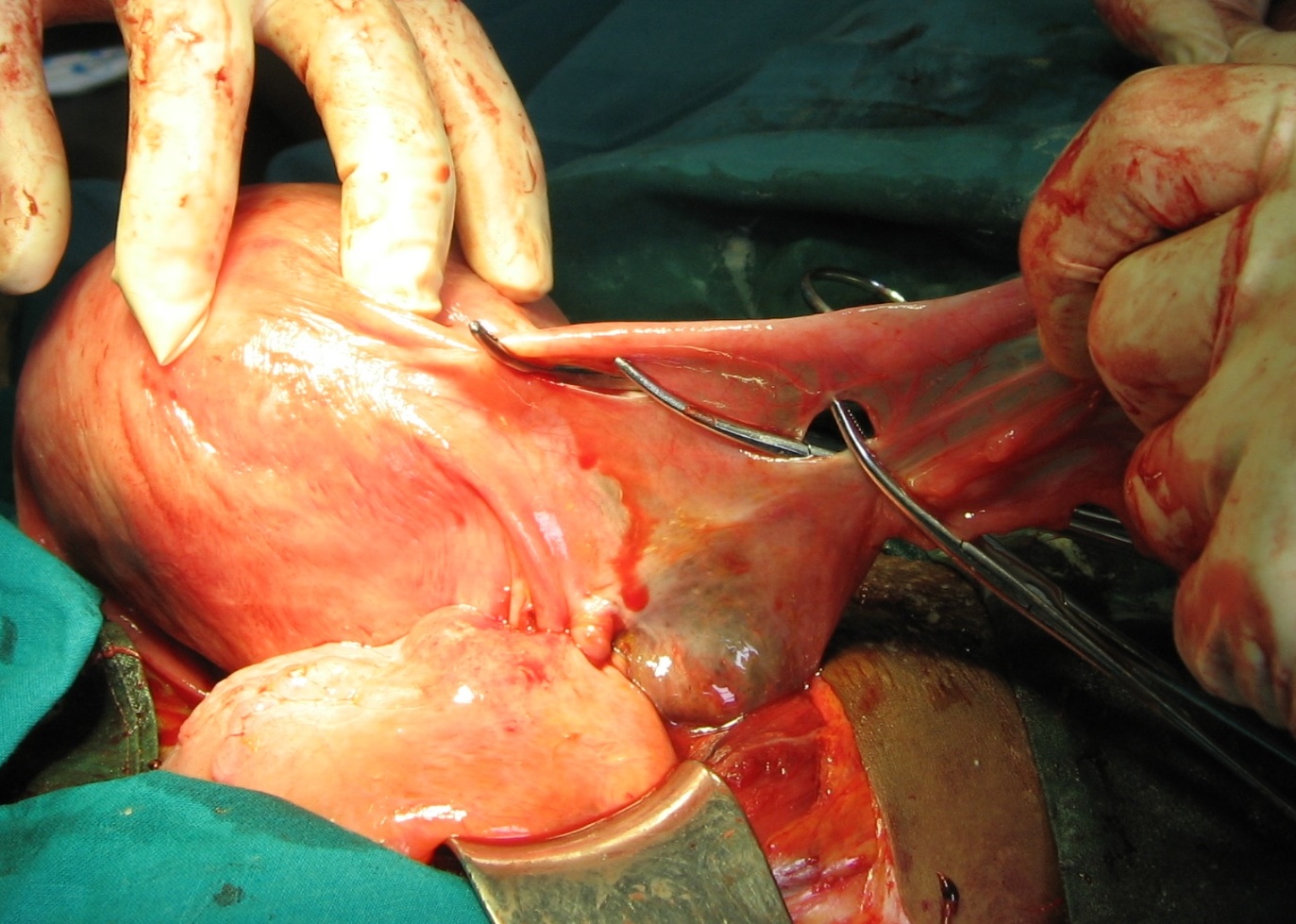
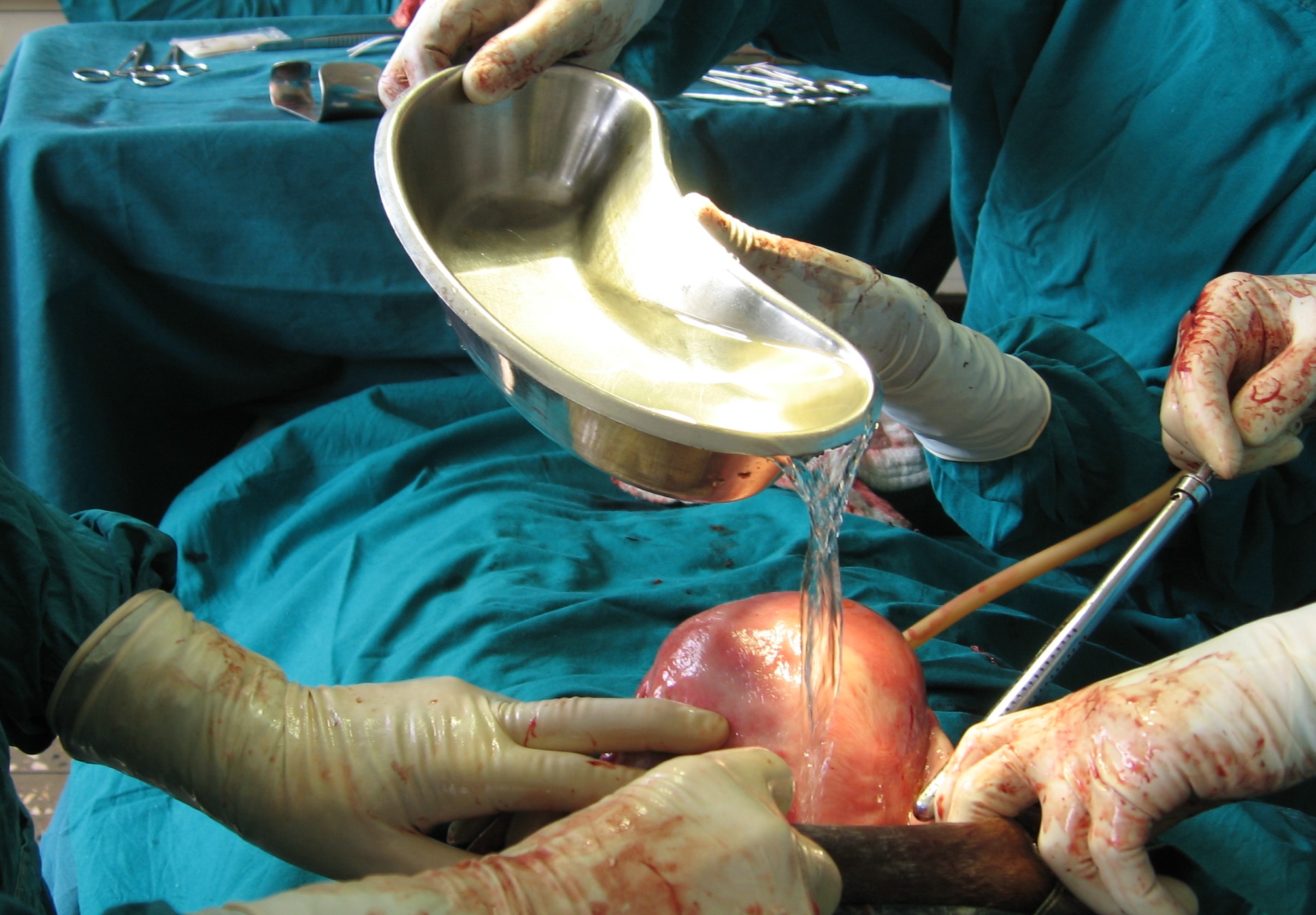
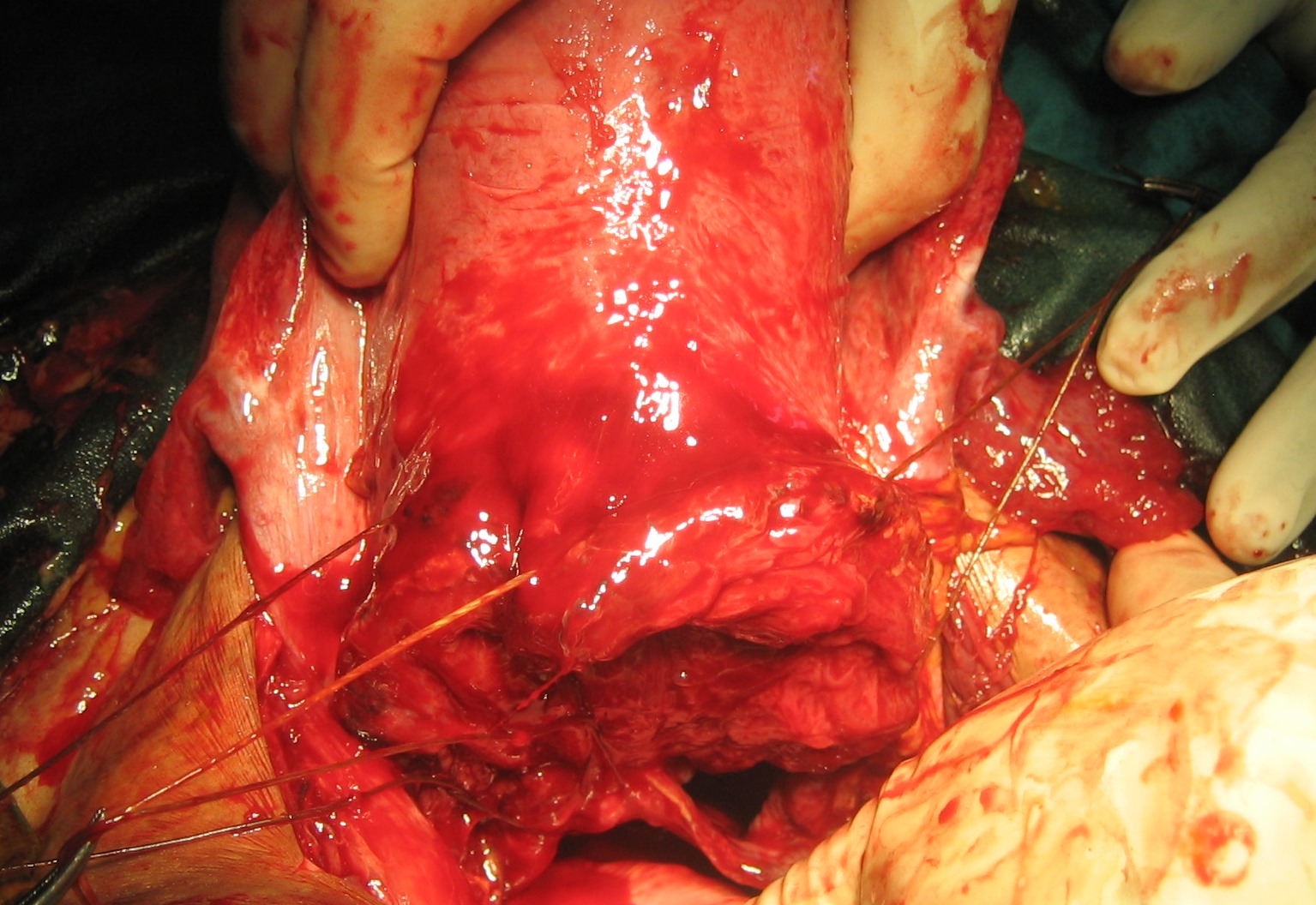
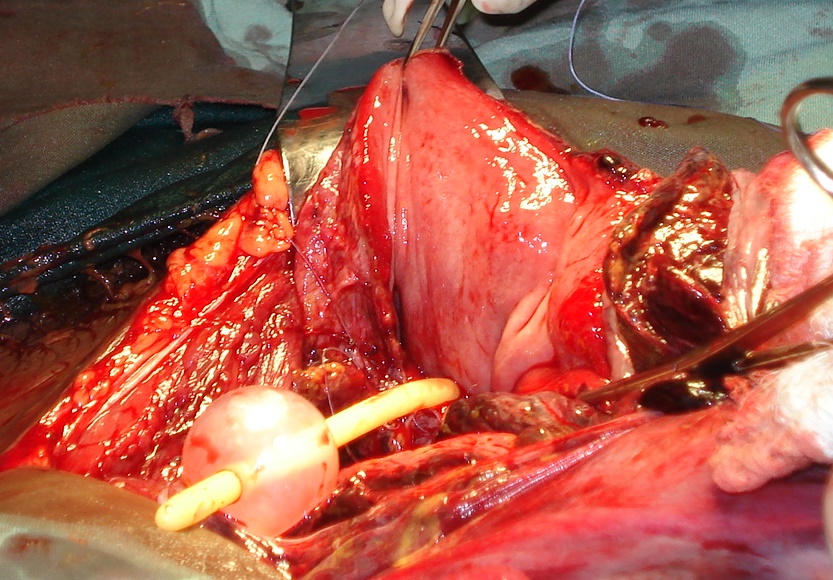
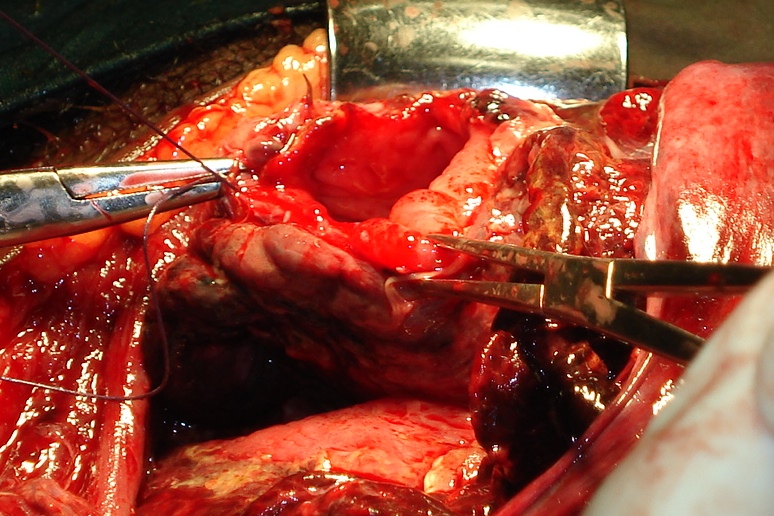
REPAIR OF RUPTURED UTERUS
SURGICAL TECHNIQUE
REPAIR OF ANTERIOR TRANSVERSE UTERINE RUPTURE














REPAIR OF LATERAL UTERINE RUPTURE









REPAIR OF POSTERIOR LONGITUDINAL


REPAIR OF POSTERIOR TRANSVERSE RUPTURE



REPAIR OF RUPTURED BLADDER
Bloody urine raises the suspicion of bladder involvement


SURGICAL TECHNIQUE










Using these principles resulted in the present maternal mortality of less than 3 % in Aira Hospital as seen in the presentation below. One of the two deceased patients in the material expired before reaching the operating theater. The maternal survival rate after surgery is thus 98.6 % and mortality with surgical treatment 1,4 %
An improvement from 5% mortality previous 10 years
An improvement from the 5 % mortality rate during the preceding 10 years.